8 Early Signs and Symptoms of Heart Failure
Early signs and symptoms of congestive heart failure include:
- Shortness of breath when lying down
- Fatigue
- Exercise intolerance
- Leg swelling
- Weight gain
- Urinating frequently

People with congestive heart failure sometimes do not suspect a problem with their heart or have symptoms that may not obviously be from the heart.

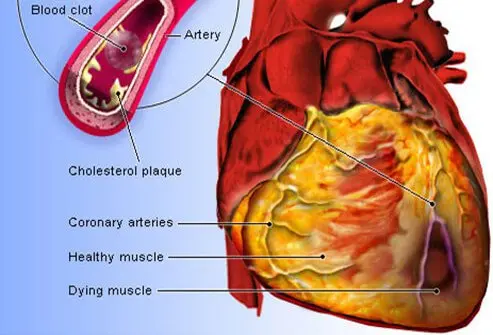
Congestive heart failure (CHF) is a syndrome that can be brought about by several causes. Congestive heart failure is a weakening of the heart caused by an underlying heart or blood vessel problem, or a combination of several different problems, including the following:
There are over a hundred other less common causes of heart failure, which include a variety of infections, exposures (such as radiation or chemotherapy), endocrine disorders (including thyroid disorders), complications of other diseases, toxic effects, and genetic predisposition. However, the cause of congestive heart failure is often idiopathic, or unknown. People who have diabetes are at increased risk for both ischemic and nonischemic heart failure.
Congestive heart failure may be exacerbated by the following lifestyle habits:
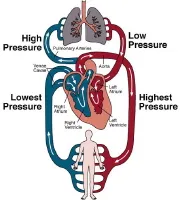
Whether through disease and/or complicating lifestyle choices, the pumping action of the heart can be impaired by several physiologic mechanisms:
Once a diagnosis of heart failure is established, evaluation of heart failure is important. Providing a complete and accurate history of symptoms is essential. Two major groups have established various stages of congestive heart failure.
The American College of Cardiology/American Heart Association stages patients according to the progression of their heart failure. The stages are as follows:
The New York Heart Association classifies patients based on their physical limitations. Classifications are as follows:
Based on a clinical study, it was determined that one in every five people will develop heart failure in his or her lifetime. Some of the most common risk factors for heart failure include the following:
Often cardiologists, who specialize in heart failure, can work together with primary care doctors and other health care providers to diagnose and treat congestive heart failure. Certain symptoms need to be checked by a doctor. If a person has any of the symptoms listed below, they should call their health care provider for an appointment. If symptoms listed below are severe or of sudden onset, seek immediate emergency care.
Other, more subtle symptoms of heart failure that are also seen in other diseases warrant a visit to a health care provider, especially if linked to any of the symptoms already listed above. These include:
Always take chest pain seriously. Congestive heart failure, per se, usually does not cause chest pain. However, remember other serious conditions that cause chest pain, such as angina and myocardial infarction, can coexist with heart failure.
If these symptoms develop quickly or worsen rapidly, seek emergency treatment.
Congestive heart failure CHF can be confused with other illnesses that cause breathing difficulties, such as bronchitis, pneumonia, emphysema, and asthma. Talking to a medical professional, along with receiving a physical exam and tests available only at a medical office or hospital, are necessary to make an definitive diagnosis. Some of the most useful tests are mentioned below.
Chest X-ray: This is very helpful in identifying the buildup of fluid in the lungs. Also, the heart usually enlarges in congestive heart failure, and this may be visible on the X-ray film. In addition, other disorders may be diagnosed.
Blood tests: People may have blood drawn for lab tests.
Echocardiogram (echo): This is a type of ultrasound that shows the beating of the heart and the various cardiac structures. It is safe, painless, and one of the most important tests for diagnosing and following patients with heart failure over time.
Stress testing: A treadmill or medication (nonwalking) stress test is used to help evaluate the cause or causes of heart failure, in particular, regarding coronary artery disease. This test is frequently combined with nuclear imaging or echocardiography to improve accuracy. Stress testing is commonly performed and is a cornerstone of diagnostic cardiology.
MRI (Magnetic resonance imaging):
Cardiac catheterization (cath): During this procedure, a small tube is inserted into and artery in the leg or arm. The catheter is moved to the heart to measure pressures inside the heart and to put contrast into the coronary arteries to look for blockages.
The treatment of heart failure depends on the exact cause, but it can usually be treated effectively. The overall goals are to correct underlying causes, to relieve symptoms, and to prevent worsening of the condition. Symptoms are relieved by removing excess fluid from the body, improving blood flow, improving heart muscle function, and increasing delivery of oxygen to the body tissues. This can be done by the various congestive heart failure treatments listed in this sections.
If the underlying cause of heart failure is not correctable by surgery or catheterization procedures, medical treatment is composed of lifestyle changes and medications.
Lifestyle changes recommended by your doctor or other health care professional can help relieve symptoms, slow the progression of heart failure, and improve one's quality of life. Lifestyle changes that may be helpful in preventing or relieving heart failure include those recommended by the American Heart Association and other organizations as part of a heart-healthy lifestyle.
Treat swelling with the following measures:
Avoid the following:
Patients with congestive heart failure should know the following information that may apply to their disease:
Medications help control both the underlying causes of heart failure and the symptoms. Medications are the most critical part of therapy for heart failure. Usually, several types of medications are required to address as many of the physiologic imbalances as possible.
People with heart failure usually take several different medications that work in different ways to lessen heart failure symptoms, to prevent worsening of the underlying disease, and to prolong life.
Diuretics (water pills): The buildup of fluid is usually treated with a diuretic.
Vasodilators: These medications enlarge the small arteries or arterioles, which relieve the systolic workload of the left ventricle. Therefore, the heart has to work less to pump blood through the arteries. This also generally lowers blood pressure. Just as importantly, they reduce the levels of certain deleterious hormones and signals that can worsen heart failure.
Nitrates are venous vasodilators that include isosorbide mononitrate (Imdur) and isosorbide dinitrate (Isordil). They are commonly used in combination with an arterial vasodilator, such as hydralazine (see below).
Hydralazine (Apresoline) is a smooth muscle arterial vasodilator that may be used for congestive heart failure. Clinical trial data has shown hydralazine plus nitrates to be especially effective in African-Americans with heart failure, when used in addition to ACE inhibitors or ARBs.
Beta-blockers: These drugs slow down the heart rate, lower blood pressure, and have a direct effect on the heart muscle to lessen the workload of the heart. Specific beta-blockers, such as carvedilol (Coreg) and long-acting metoprolol (Toprol XL), have been shown to decrease symptoms, hospitalization due to congestive heart failure, and deaths. Other beta-blockers include bispropolol (Zebeta), atenolol (Tenormin), propranolol (Inderal), and bystolic (Nebivolol), but they are generally not used with significant congestive heart failure.
Inotropes: IV inotropes are stimulants, such as dobutamine and milrinone, which increase the pumping ability of the heart. These are used as a temporary support of a very weak left ventricle that is not responding to standard congestive heart failure therapy. Commonly used inotropes are dobutamine (Dobutex) and milrinone (Primacor). Phenylephrine (Neo-Synephrine) may be used when a patient is suffering with severe low blood pressure.
ACE inhibitors and ARBs may cause the body to retain potassium, but this is generally only a problem in people with significant kidney disease, or in people who are also taking a potassium-sparing diuretic, such as triamterene or spironolactone. Potassium levels can be monitored with lab testing.
Calcium channel blockers (CCBs) are arterial vasodilators that are not used for treatment of heart failure because clinical trials have proven no specific benefit. However, calcium channel blockers are useful for lowering blood pressure. If the cause of the congestive heart failure is high blood pressure and the patient is not responding to ACE inhibitors or ARBs, a CCB may be considered. Some CCBs include diltiazem (Cardizem), verapamil (Calan, Isoptin), nifedipine (Procardia, Adalat), and amlodipine (Norvasc).
These above-mentioned medications can be very effective in treatment of patients with systolic heart failure. There are not many successful therapies proven with clinical trial results available for patients with diastolic heart failure. Patients with diastolic heart failure are often prescribed these medications to treat their underlying conditions, such as hypertension or coronary disease, and as an extrapolation of favorable results, in the treatment of systolic heart failure. Several clinical trials are ongoing.
The medications listed above are very commonly used, but other mediations may be prescribed depending on the underlying cause of the heart failure or medical condition.
Getting the most out of congestive heart failure medications involves the following:
Other treatments or procedures may be offered, depending on the underlying cause of the heart failure.
Angioplasty: This is an alternative to coronary bypass surgery for some people whose heart failure is caused by coronary artery disease and may be compounded by heart damage or a previous heart attack. Angioplasty is performed to treat narrowing or blockage of a coronary artery that supplies the left ventricle with blood. The narrowing or blockage is caused by cholesterol deposits.
Pacemaker: This device controls the rate of the heartbeat. A pacemaker may keep the heart from going too slow, increasing heart rate when the heart is not increasing enough with activity. It also helps sustain regular rates when the heart is not beating in a coordinated way. Or, the pacemaker performs some combination of these.
Implantable cardioverter defibrillator (ICD): This device returns the heart to a normal rhythm by pacing or delivering an electrical shock, with a life-threatening arrhythmia.
Cardiac resynchronization therapy (CRT): This involves a biventricular pacemaker that is used to synchronize the pumping action of the left and right ventricles. Synchronization improves the effectiveness of the heart as a pump since with heart failure the pumping action is sometimes uncoordinated.
Temporary cardiac support: An intra-aortic balloon pump is used as temporary support for left ventricle function, such as in a large heart attack, waiting for the heart to recover. There are other similar devices that can be used to temporarily support the heart if there is something that can be done for the underlying heart failure.
Surgery can repair some underlying causes of heart failure, such as blockage of the coronary arteries, a valve problem, a congenital heart defect, or thickened pericardium. For patients with severe coronary artery disease, coronary artery bypass graft (CABG) surgery can be conducted to circumvent blockages in vessels and ensure that the heart muscle maintains its blood supply. Valve replacement surgery can also be performed to repair malfunctioning heart valves. However, once the heart's ability to pump blood is severely, permanently, and irreversibly impaired, no surgery can repair the damage. The only alternative is a heart transplant. This option is for patients who are not elderly and who do not have other medical conditions that would make it unlikely for a heart transplant to be successful. Heart transplant evaluations are done in specialized centers. Over the years there have been new innovations in the field of cardiac surgery and if a heart transplant is not available, a left ventricular assist device (LVAD) may be implanted to help prolong life.
Left ventricle assist device (LVAD): This device is surgically implanted to mechanically bypass the left ventricle. It can be used as a “bridge to transplant” until a heart transplant is available.
Total artificial heart (TAH): For patients with severe, end-stage heart failure.
Congestive Heart Failure Follow-up
If a patient has congestive heart failure, he or she will need frequent, regular medical attention to adjust medications and watch for side effects. Keep scheduled regular visits with the health care provider, as he or she recommends, because congestive heart failure is a serious medical condition that requires constant monitoring. Patients need to educate themselves as much as possible about this life-threatening condition and follow the suggestions below:
Congestive heart failure can be the ultimate result of a number of diseases, or lifestyle choices, that damage the heart. Some of these can be prevented. Others cannot be prevented but can be treated successfully.
Some examples of illnesses or lifestyle choices that can lead to congestive heart failure are as follows:
In some cases, a family history of heart failure can be present. Many cases are a combination of factors, and in other cases, the cause is unknown.
If a person has congestive heart failure, they are at increased risk of developing pneumonia. They probably should receive both the pneumonia vaccination and annual flu shots. Patients should ask their doctor or other health care professional to be sure.
Heart failure is a major health problem that comes with the aging of America. Today, many more people are surviving heart attacks and other heart diseases. Enduring these heart conditions allows them many more years of quality life, but can eventually lead to the development of heart failure.
In recent years, more effective medications have been developed that improve the outlook of heart failure. Medications are the mainstay of therapy with congestive heart failure.Having the support of doctors and other health care professionals, family, friends, and caregivers is essential to effectively coordinate all of the needs of a person with heart failure.
People with severe heart failure have special needs beyond standard medical care.
Early signs and symptoms of congestive heart failure include:
